| Approximately
one in a thousand children aged 0-16 years is visually impaired. This represented
50 children in an average health district with a population of 250,000
(1), a significant proportion of whom has cerebral vision impairment.
Children
with multiple disabilities are frequently referred for refraction and assessment
of visual function, so that parents and carers can be advised about and
understand what the child can and cannot see. The aim of this article is
to outline the principle visual problems and to suggest approaches to their
management.
 Assessment
of vision Assessment
of vision
The goals
of assessment are to determine the functional vision available for communication,
education, navigation and other activities, and to advise on methods of
enhancement and compensation to circumvent the visual problems and enhance
development for each individual child.
History
A detailed
history can help compensate for what may necessarily be a limited examination
in these children.
The
profoundly visually impaired child may show evidence of "blind sight" subserved
by the collicular visual system (2, 3). Such children commonly have impaired
movement of all four limbs and appear to react to slowly moving targets
at the side. If they are mobile, they can navigate around obstacles, but
paradoxically may show little evidence of other visual functions.
Severe
visual impairment warrants particular enquiry concerning eye contact, and
the maximum distance from which a silent smile is returned.
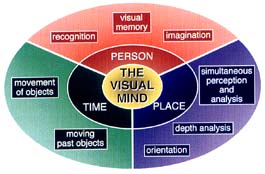
Vision
with an acuity of 6/60 or better necessitates questions directed towards
identifying the following problems (fig 1 above). (4, 5).
Estimating
Visual Function
Function
assessment is carried out with both eyes open.
Visual
behaviour is watched carefully. If the child makes eye contact, move back
gradually until it is lost, in order to establish the distance within which
communication must be made. The fixation pattern if the child looks around
is informative. An alert child repeatedly changes the direction of gaze
to fixate on different targets, whereas the child with impaired vision
appears to look past the examiner with inaccurate and less frequent eye
movements.
Visual
acuity may be estimated in a number of ways, the functional significance
of which needs to be distinguished.
-
VEP
acuity is the minimum target separation which permits VEP signal detection.
-
Detection
acuity (Catford drum or Stycar balls) estimates the minimum size visible.
-
Resolution
acuity (preferential looking cards) is the minimum separation which
allows discrimination.
-
Recognition
acuity (letters or pictures) is the minimum size which facilitates
identification.
Tests
must be appropriate for age and ability. Cardiff cards afford a
rapid and reproducible preferential looking test. The vertical presentation
is helpful in obviating problems due to hemianopia or horizontal nystagmus
and the picture format allows end point detection. Keeler cards
are more suitable for infants who are severely impaired, and may need to
be presented vertically if hemianopia is present or suspected. Recognition
tests can give a lower visual acuity due to crowding.
As
the visual acuity is a measure at maximum contrast and does not estimate
functional vision, the size of educational material must be gauged to allow
maximum speeds of access to information.
Contrast
sensitivity may be estimated using fading optotypes or in younger children,
low contrast faces revealed from behind a cover*. Reduced contrast sensitivity
necessitates the use of high contrast educational material.
Colour
vision is commonly intact although some children can match but not name
colours (colour anomia).
Functional
visual field assessment is carried out binocularly, particularly to elicit
homonymous defects. For the young child, the child's attention is attracted
while a target is introduced from behind in each of the four quadrants,
anticipating a head turn.
For
the older, co-operative child small discreet movements of an extended forefinger
in each of the four quadrants, both singly and on both sides simultaneously,
can be made into a game. Homonymous defects are commonly identified. Inattention
(extinction) is common and functionally can be equally handicapping, e.g.
when crossing roads or attempting to read as the page progressively disappears
for a left hemianopia and jumps into view if it is on the right.
Eye
movement disturbances are common. These include nystagmus (particularly
with additional optic nerve hypoplasia), gaze palsies, oculomotor apraxia
and impaired tracking. The latter may cause children to have no interest
in fast moving cartoons but to prefer TV programmes with limited movement.
Accommodation
and convergence. Some children with brain damage have reduced or absent
accommodation and therefore poor third dimensional tracking which leads
to difficulty overcoming hypermetropia. Retinoscopy prior to cycloplegia
can identify impaired accommodation and reveal manifest hypermetropia not
corrected by the accommodative reflex. The provision of spectacles can
give gratifying results.
Identification
of Higher Visual Processing Disorders
Observation
and a thorough history may reveal and help explain some of the following
types of visual problem (see fig 1).
-
Simultaneous
visual processing problems (9) are common in children with impaired
movement of all four limbs and may manifest as difficulty in finding a
toy on a patterned carpet. Crowding is a clinical manifestation of the
disorder (6). Sorting out a complex visual scene can take a long time.
Such children may read short words easily but can lose track with long
words (4). Enlargement and simplification of educational material, with
sequential presentation against a plain background can be recommended.
-
Recognition
of people, shapes or objects can be selectively impaired particularly in
periventrical leucomalacia (4). A child may be able to see a small toy
in the distance but be unable to recognise a close relative in a group.
Affected children compensate by voice recognition or by recognising shoes
or brooches.
-
Problems
with reading are best assessed by an expert in visual impairment and
education who takes into account the optimal size and lighting required
for a maximum comfortable reading speed and who recognises the nature of
specific reading disorders.
-
Problems
with orientation occur (5) but are not just visual in origin. Children
blind from eye disease can be adept at navigation, while children with
posterior cerebral pathology (particularly on the right) may have good
acuity but get lost and cannot find their toys. Limited mobility and constant
supervision do not give opportunities to develop navigational skills. Education
strategies and mobility training which compensate by using, for example,
language memory for standard routes, are essential.
-
Perception
of movement is most commonly impaired on account of impaired tracking,
but can rarely be a problem in children with damage to the part of the
brain responsible for movement perception, area V5 (5.10).
-
Visual
memory is used for copying tasks which can prove difficult for children
with cerebral visual impairment. In new environments, affected young children
may have impaired face recognition and navigation.
-
Visual
imagination is also observed by the occipital brain, and descriptions
given by parents may indicate good language processing, but difficulties
in handling imagined visual concepts.
-
Lack
of visual attention which is intermittent is common when tiredness,
pre-occupation or distraction lead to behavioural diminution of visual
function. In contract, familiarity with the environment appears to enhance
visual performance.
-
Prolongation
of visual tasks is a common feature. Sufficient time should be given
for a child to demonstrate his or her ability, and the reduced performance
speed recognised.
Profoundly
disabled children may suffer from any of the above problems, but lack of
communication can render it impossible to delineate specific deficiencies.
Conclusion
Vision
Assessment Teams probably provide an optimal service (1). The majority
of such children undergo gradual visual improvement with time, but early
intervention programmes can favourably affect the visual development of
young children with cortical visual impairment. (11-13).
A report
summarising the visual abilities and disabilities with recommendations
for developmental and educational material approaches and, written in plain
English for the parents to give to carers and teachers can be very helpful
in providing a structured addition to the care plan.
Prof
G N Dutton
References
(1) The
Royal College of Ophthalmologists & the British Paediatric Association.
(1994). Ophthalmic services for children. A report of a joint working
party. Services for children who are partially sighted or blind. R.
C. Ophth. BPA. London. pp. 13-14.
(2)
Haigh D. (1993). Chronic disorders of childhood. In: Visual problems
in childhood. Ed: Buckingham T. Butterworth-Heineman Ltd., Oxford.
pp. 47-62.
(3)
Jan JE., Wong PKH., Groenwell M., Flodmark O., Hoyt CS. Travel vision
"Collicular visual system?" Pediatr. Neurol. 1986. 2: 359-62
(4)
Jacobson L., Ek U., Fernell E., Flodmark O., Broberger U. Visual impairment
in preterm children with periventricular leukomalacia - visual, cognitive
& neuropaediatric characteristics related to cerebral imaging.
Devel. Med. Child Neurol. 1996. 38: 724-735.
(5)
Dutton G., Ballantyne J., Boyd G., Bradnam M., Day R., McCulloch D., Mackie
R., Phillips S., Saunders K. Cortical visual dysfunction in children:
a clinical study. Eye 1996. 10: 302-309.
(6)
Pike MG., Holmstrom G., de Vries LS., Pennock JM., Drew KJ., Sonksen PM,
Dubowitz LMS. Patterns of visual impairment associated with lesions
of the pre-term infant brain. Devel. Med. Child Neurol. 1994. 36: 849-862.
(7)
Mercuri E., Atkinson J., Braddick O., Anker S., Nokes L., Cowan F., Rutherford
M., Pennock J., Dubowitz L. Visual function and perinatal focal cerebral
infarction. Arch. Dis. Child 1996. 75: F76-F81.
(8)
Harvey EM., Dobson V., Luna B., Scher MS. Grating and visual field development
in children with intra-ventrical haemorrhage. Devel. Med. Child Neurol.
1997. 39: 305-312.
(9)
Foley J. Central visual disturbances. Devel. Med. Child Neurol.
1987. 29: 116-120.
(10)
Ahmed M., Dutton GN. Cognitive visual dysfunction in a child with cerebral
damage. Devel. Med. Child Neurol. 1996. 38: 736-743.
(11)
Jan J., Sykanda A., Groenveld M. Habilitation and rehabilitation of
visually impaired and blind children. Paediatrician 1990. 17: 202-207.
(12)
Sonksen P.M. Promotion and visual development of severely visually impaired
babies: evaluation of a developmentally based program. Devel. Med.
Child Neurol. 1991. 33: 320-335.
(13)
Sonksen P., Stiff B. Show Me What My Friends Can See. 1991: John
Brown Ltd., Nottingham.
* Available
from Precision Vision, 745 North Harvard Avenue, Villapark, Il. 60191,
USA |